A Brief History of Electronic Health Records

Our current body of medical knowledge began with notations made by those tasked with patient care going as far back as 3,000 B.C. It wasn’t until the 1920s, however, that healthcare professionals widely came to understand the benefits of carefully documented patient health records. Initially, patient record-keeping took the form of the “Problem Oriented Medical Record” (POMR), which as the name suggests, was organized around solving medical problems, as opposed to preventing illness and maintaining optimal health.
The birth of electronic medical records
Initially all patient information was recorded on paper (or parchment, in ancient times). However, the burgeoning computer age in the mid-1960s led to the birth of the first “Electronic Medical Records” (EMRs), which were essentially the equivalent of patient “charts,” except in electronic form. EMRs were an improvement over paper records. However, technology was significantly more expensive at this time, and the utility of EMRs was limited by their inherent lack of interoperability .Interoperability, in the context of health information, refers to the seamless and secure exchange of electronic health information between authorized users of such information. In other words, interoperability is as much about sharing, as it is about protecting the privacy of, patient health data, for the benefits of both patient and provider.
The birth of HIPAA
Nevertheless, legislation introduced that would have required uniform adoption of EMRs sputtered to a dead end in Congress. On the other hand, legislation addressing privacy of patient data gained enough traction to lead to the passage of HIPAA: the Health Insurance Portability and Accountability Act (HIPAA).
When HIPAA was introduced, its primary purpose was ensuring employees would continue to receive health insurance coverage when they were between jobs (hence, “portability”). Another purpose, however, was improving efficiency in the healthcare industry (hence, “accountability”). In furtherance thereof, HIPAA took aim at the vast amounts of paperwork generated in the course of the claims process, by, among other things, requiring providers and payers to adopt standardized treatment and diagnosis codes. As a result, the adoption of HIPAA was pivotal in the move toward adopting electronic patient records.
The birth of HITECH
As much as EMRs made good sense to providers post-HIPAA, the cost of transitioning from paper was proving prohibitively expensive. Congress responded in 2009 by passing the Health Information Technology for Economic and Clinical Health Act (HITECH), which introduced incentives for providers to “go electronic.”
The birth of Electronic Health Records
Over time, but particularly in the past two to three years, HITECH has shifted the EMR paradigm entirely. The process of optimizing patient data came to focus in content as much as form. POMRs gave way to records aimed at presenting a full picture of a patient’s total health: the Electronic Health Record (EHR). EHRs are, by law, the property of the patient, and only the patient can grant power to a provider to allow access by third parties. For more information on what should generally be contained in an EHR, please visit Tell Us Where It Hurts: How Tech Can Heal Healthcare.
Still so far to go
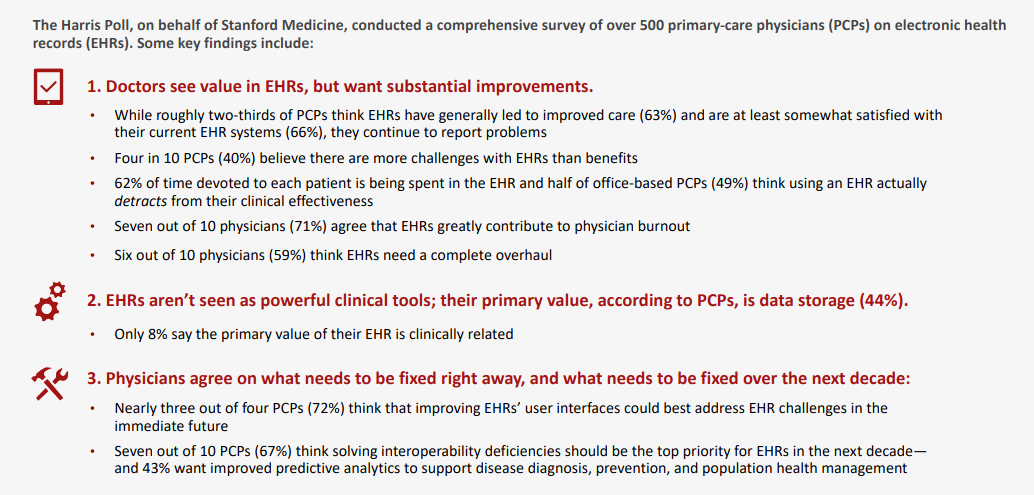
Electronic health records hold significant benefits over their predecessor systems for health information record-keeping. They hold enormous promise for addressing healthcare’s inefficiencies by turning an overabundance of underutilized data into assets that work synergistically to benefit providers, payers, and patients. However, the promise remains unfulfilled at present, in large part due to interoperability. We’ll be exploring the current state of interoperability in an upcoming post on the Exela Blog. Can’t wait? Check out the full story in our Q4 Edition of PluggedIN: Tell Us Where It Hurts: How Tech Can Heal Healthcare.
Sources:
https://www.rasmussen.edu/degrees/health-sciences/blog/health-information-management-history/
https://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2233232/
https://www.hipaajournal.com/what-is-the-hitech-act/
https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2016.1651