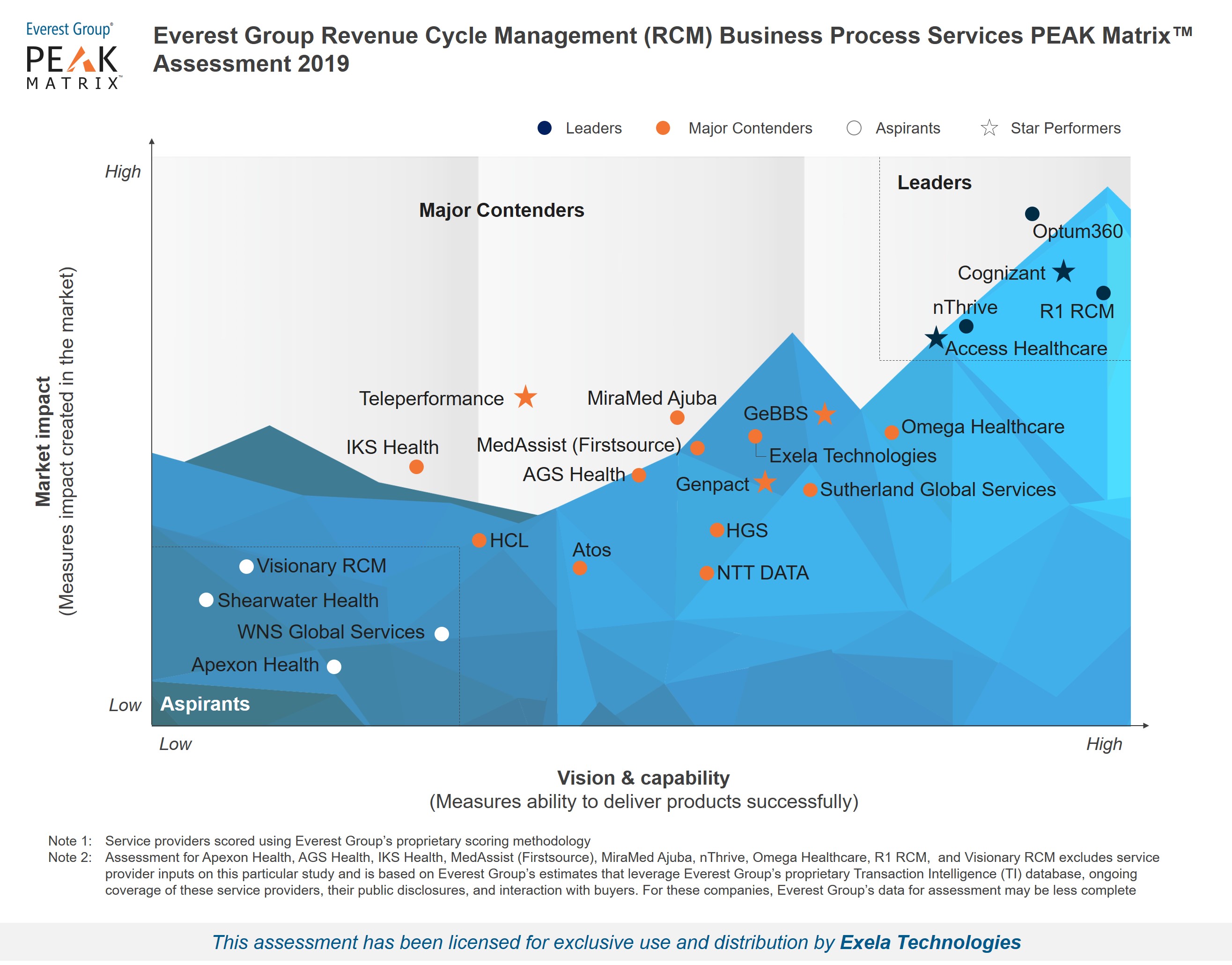
Revenue Cycle Management (RCM) Business Process Services PEAK Matrix™ Assessment 2019
Analyst quote from Manu Aggarwal, Practice Director, Everest Group:
“The US healthcare industry loses over US$250 billion annually in initial claim denials due to improper submissions. In addition to issues around interoperable systems, lack of standardized processes, limited talent availability, etc. one of the core issues that healthcare claims still get stuck around is the usage of paper-based submissions,” said Manu Aggarwal, Practice Director, Everest Group.
“In the era of digital assets, healthcare is still caught in the age-old way of submitting complex claims. Exela Technologies, via its PCH platform, aims to streamline the traditional mailroom functions of providers and convert them into data and document exchange platforms. With the ability to emulate the traditional submission workflow and EDI integrations via partners, Exela’s solution helps providers optimize their claims submissions without the need for high upfront investments in technology.”
Click here to download the full report.
