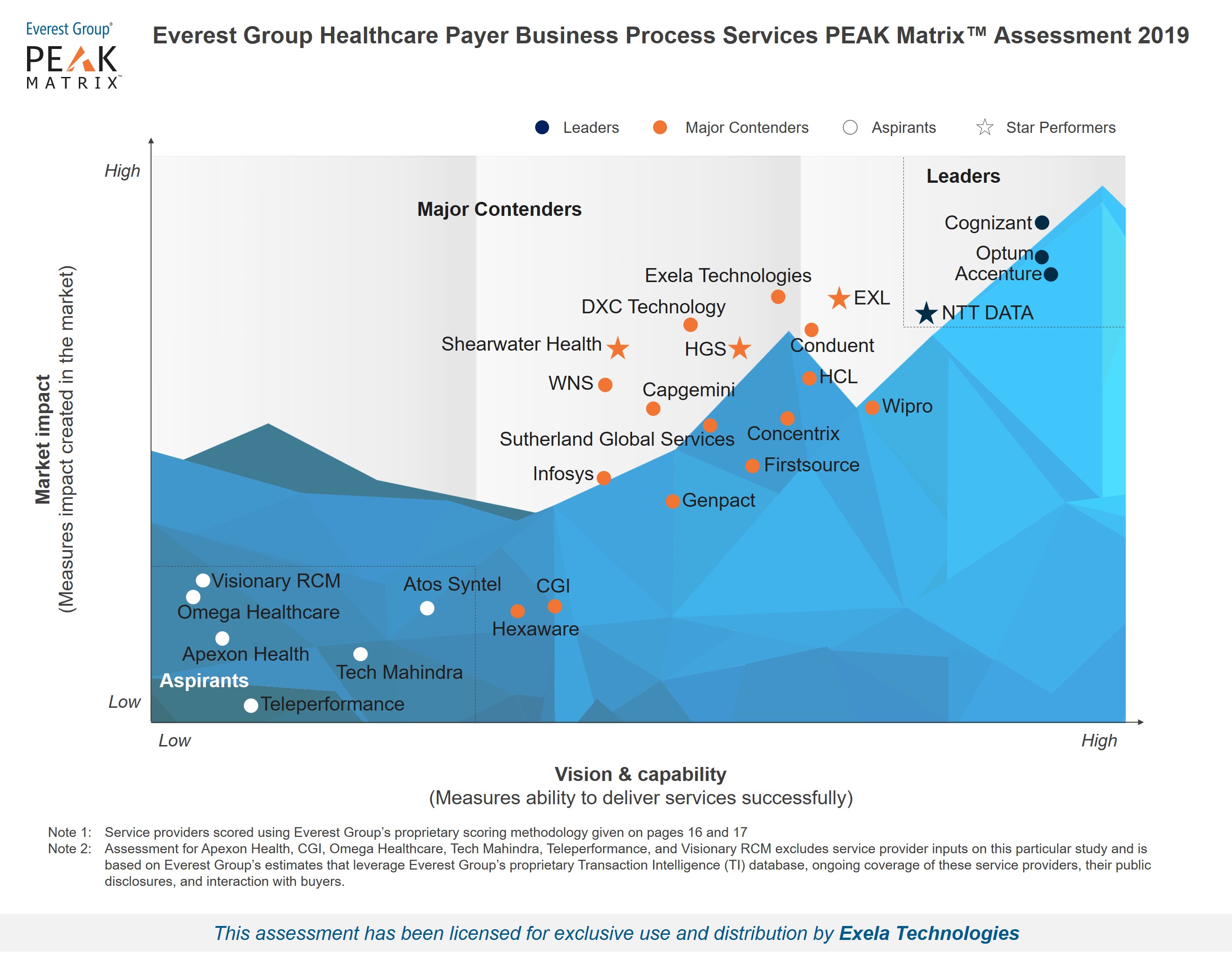
Healthcare Payer Business Process Services PEAK Matrix™ Assessment 2019
Analyst quote from Manu Aggarwal, Practice Director:
“From RCM systems to billing to clearinghouses to claims intake, the healthcare industry attracts attention from hundreds of different services and technology vendors. However, the problem of high denial rates is as bad as ever and it leads to higher costs not only for the providers but payers too – not to mention the member dissatisfaction and loss of goodwill that goes with it,” stated Manu Aggarwal, Practice Director, Everest Group. “Exela’s ability to be the bridge between providers’ billing systems and the payers’ claims intake is key to reducing instances of denials. The ability to handle complex claims, which otherwise follow a manual submission process, via its PCH offering is a unique value proposition in the industry.”
Click here to download the full report.
